introduction
Payer Contracting Strategy and Regulatory Research
SCALE Payer Contracting Strategy
SCALE Payer Contracting Strategy provides comprehensive payer consulting and contracting services. Payer strategy development identifies opportunities to improve profitability and competitive position through language provisions. Our team offers integral and insightful research to help clients make the most informed decisions for all stakeholders.
We combine decades of experience working for payers, an assertive approach, and use of our extensive industry contacts to produce best-in-class results for our clients. Our analyses include research of market dynamics, opportunities for value-based care partnerships, geographic leverage, and performance metrics to maximize the outcome of the negotiation. Our additional services that we offer provide capacity for ongoing and unforeseen payer matters as needed.
In addition, to support, organize, and manage payer contracts, we can build and implement a Contract Management Solution (CMS) tool – an easy-to-use digital repository of all payer contracts and with support for related business functions. Recurring professional services are provided to support on-going payer contract management which may include:
- Thorough contract review
- Market analysis using price transparency data
- Rate and service comparisons based on your specialty
- Contracted reimbursement and revenue modeling based on utilization
- Payer strategy development and targeted recommendations
- Collaboration and leadership during payer-provider negotiations
- Build, set – up and maintain Contract Management Solution (CMS) tool
- Contract renewal management.
- Periodic payer contract strategy development due to market or provider changes.
- Payer dispute resolution
Contract Management Solution (CMS)
- Creates single, easy to access and use digital repository for housing all payor contracts, appendices, and other related documents.
- Not person ‘dependent’.
- Easy knowledge transfer of processes, management and content.
- CMS is designed to easily capture metadata about contracts: key terms,
pricing, notification protocols, critical dates, coverage, etc. - Detailed User Guide and technical documentation provided.
Users can set-up ‘action’ alert reminders such as 90-days from renewal date, need to schedule penetration test, get updated SOC audit, etc.
- Report writer equips users with ability to generate a variety of pre-defined reports or export data into Excel or CSV file.
- Discussion Tracker enables capture of user comments and discussion related to contract review and approval process.
Built-in tracker log provides audit/ checkpoint functions to ensure all appropriate reviews are made and sign- offs are secured.
Secure application with admin oversight module to define which users have access rights to view/read/write.
Secure Access
PDFs of all Contracts/appendices
Admin Functions
Admin Functions
MS Outlook Interface
Meta Data
Export Data
Export Contracts
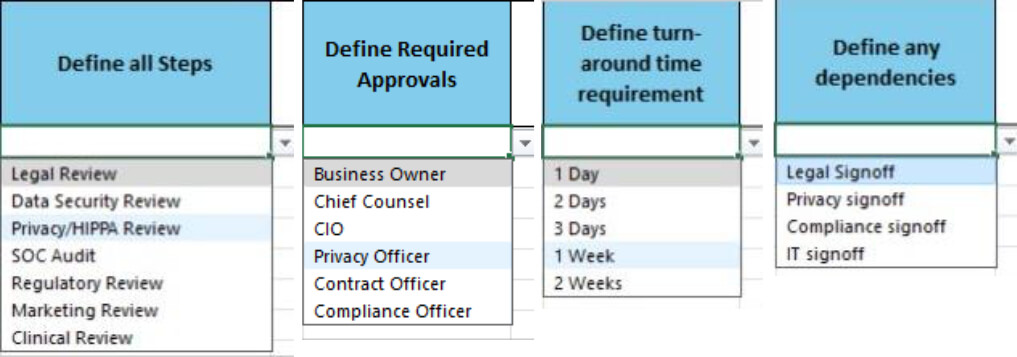
Contract Approval Sequencer
Define critical path sequence to secure review & sign-off of all required stakeholders. This intelligent approval sequencer enables users to:
- Define all required steps
- Define required approvals
- Define turn-around requirements
- Define any dependencies
- Assign due dates
- Track contract completion review status
Simplify the oversight and management of all payor contracts
Repository of unlimited payor contracts, amendments, and attachments such as NDA, BAA, Performance Guarantees, etc.
Links/tags for cross-referencing critical terms, pricing, effective/ expiration/recurring dates, etc.
Documents in PDFformat, convertible to Word.

Smart data entry interface prompts for key terms, conditions, critical dates, required signatories, etc.
Ability to add custom fields.

HIPPA compliant
2-factor authentication and e-signature.
Configurable user roles and permissions.
Enable users to define a custom contract sign-off sequence, including specification of dependencies and turnaround time frames.

Application integrated with MS Outlook.
Enables triggers to sent ‘Action Needed’ alert emails.
Compose, sent and receive contract related emails.
Captures user comments related to contract provisions and approval process review.
SCALE Regulatory Research
SCALE’s Payer and Regulatory Research services examine CMS trends, Congressional legislation, and value-based care innovations to inform your business. Additionally, we provide landscape analyses that identify opportunities in healthcare across the country, offering integral and insightful research to make the most informed business and investment decisions. Clients can utilize our research capabilities when considering expansion into new markets through de novo clinics, acquisitions, or when evaluating the impact of new healthcare policies.
Client Profile
-
Services Deployed:
MSO & Practice Integration
Payer Strategy -
Specialty:
Orthopedic
CASE STUDY:
Orthopedic MSO Case Study – Payer Contracting Strategy
SCALE was engaged by an orthopedic Management Services Organization (MSO) group to assist with payer contract review, contract strategy development, and contract renegotiation with multiple payers across their Commercial and Medicare Advantage (MA) lines of business.
What Our Client Partners Say
Check out our White Paper: CMS Behavioral Health Program Brings Value-based Care and Health Equity to Mental Health Practices
SCALE Payer Contracting Strategy and Regulatory Research benefits from the extensive collective experience of our seasoned team of healthcare operators, leaders, and executives, providing our clients with an exclusive insider's perspective on the challenges and opportunities healthcare businesses face across the spectrum.
The SCALE Difference
We utilize our extensive national network to give our clients an accurate outlook and overview before deploying capital and making acquisitions in targeted regions.
Payer Research
The payer landscape can vary greatly between states. Our understanding of how payers work in different regions gives our clients an accurate understanding of the possible opportunities and challenges when forming a provider group strategy.
Employers
Employers and employer-sponsored health plans can drive growth in a healthcare market and create new business opportunities. We can help identify partnerships with employers for our clients and project an employer’s total effect on the market.
Competitive Analysis
Understanding your competitors, their services, and the market patient/client population allows for greater ability to adapt to changes in the market and strategize for the future.
Data and Analytics
SCALE utilizes commercial payer data from over 100 million covered lives, employer sponsored plans, and published state and federal reimbursement data. We combine our analysis of the data with interviews and surveys to give our clients a well-rounded view of the market.
Patient / Client Opportunities
We combine use of data with surveys and interviews to estimate opportunities with the current patient population and areas for future growth.
Regulation / Policy / Legislation
Government regulations and legislation can be a obstacle to account for in the future but also create opportunities in the market. Our deep experience with analyzing healthcare reforms allows SCALE to give an accurate view of the current environment and likely outcomes.